Summary
Researchers and clinicians from Maastricht University and other prestigious academic and clinical institutes started a new important social media initiative aiming to facilitate the free and full open access to latest scientific publications regarding the clinical efficacy, safety, and application expansion of noninvasive brain stimulation (TMS and TES).
This initiative is relevant and timely. Noninvasive brain stimulation is among the most dynamically developing fields in clinical brain research with a constant stream of innovation. Thousands of new scientific articles are published each year describing new insights and improved protocols and procedures for applying Transcranial Magnetic Stimulation (TMS) and/or Transcranial Electric Stimulation (TES), with many of these innovations being directly relevant for clinical practice.
At the same time, the official recognition and approval of TMS (and in some countries also TES) as a clinically effective treatment for various neuropsychiatric disorders such as depression or OCD has led to a constant increase in the number of clinicians successfully offering TMS or TES treatment services to their patients, often in private practices, small clinics, or non-academic hospitals.
While this increasing worldwide adoption of TMS and TES in clinical practice is great news for both, patients and the mental health care system, it also creates a new challenge.
Most of these TMS practitioners don’t have free and open access to these new scientific articles published in subscribed journals, nor do they have the time to scan the overwhelming number of new articles for scientific quality and clinical relevance. These clinical colleagues are also not always attending the scientific conferences where new developments are presented and discussed.
To address this increasing gap between scientific research and clinical practice in the field of noninvasive brain stimulation, the International Clinical TMS Certification Course LinkedIn page was created, providing simple access to relevant scientific publications from the international brain stimulation literature and inform about new developments relevant for the clinical use of TMS and TES. The explicit aim is to keep researchers, clinical practitioners, health care professionals, but also patients, informed about latest scientific developments in the field.
Since February 2023, everyone interested can now simply follow the International Clinical TMS Certification Course on LinkedIn to benefit from this service and to stay connected with the scientific research in the field of TMS and TES.
You can follow this initiative here.
Background
Neuroscience has impact
The decade of the brain has seen a revolution in empirical brain research, mainly fueled by the development of new noninvasive brain imaging and brain stimulation technologies. Based on these new methods, progress in neuroscience has continued relentlessly. Although we still have a long way to go to understand many of the basic mechanisms of how our brain works, let alone what exactly goes wrong in the brain when suffering from a neuropsychiatric disorder, the number of meaningful breakthroughs and neuroscience publications have only grown and started to have a measurable impact on how we understand, define, diagnose, and even treat mental health diseases as brain-based disorders.
Non-invasive brain stimulation (NIBS) is probably the prime example of how neuroscience research leads to a successful clinical application impacting the life of thousands of patients worldwide every day. After more than 30 years of basic NIBS research, treatment of depression and other neuropsychiatric disorders with commercially available transcranial brain stimulation devices is now established, regulatorily approved, and reimbursed (in many countries) and the question is no longer whether such treatment is effective, but rather whether it should be considered as a first-line or even first-choice treatment. But despite this great achievement and long journey from basic science in the lab to regular mental health care programs in the clinic, the field is still progressing at unreduced speed with ever new and further optimized protocols and procedures being introduced every year. By now, NIBS techniques have successfully demonstrated equivalent or even superior effects relative to alternative (e.g. drug) treatments of certain brain-based disorders, with only minimal side effects (1-8).
Non-invasive brain stimulation techniques (NIBS)
Non-invasive brain stimulation (NIBS) is an umbrella term for all sorts of transcranial brain stimulation or neuromodulation tools. Transcranial brain stimulation implies that the technology uses different modalities to change brain activity through the intact skull (transcranial) which makes transcranial and non-invasive brain stimulation synonyms for the same principle. Currently, the clinically most established and well-known non-invasive brain stimulation techniques are transcranial magnetic stimulation (TMS) and transcranial electric stimulation (TES), the latter often also referred to as low-intensity or low-output TES (LOTES). In TMS, a time-varying magnetic field is applied via an electromagnetic coil placed on the scalp of the patient. This time-varying magnetic field induces a spatially varying electric field in the brain, causing an electromotive force capable of depolarizing cortical neurons based on principles of electromagnetic induction. TES, in contrast, uses a set of two (or more) electrodes where a low intensity current flows from the anode electrode to the cathode electrode, thereby modulating the underlying cortical tissue. TES can be applied in the form of transcranial direct current stimulation (TDCS) or transcranial alternative current stimulation (TACS). Unlike TMS, TES mostly does not depolarize neurons but instead changes the resting membrane potential, thereby modulating the excitability and reactivity of the stimulated brain region. Also, while TMS uses magnetic fields that are not spatially distorted when targeting a certain brain region offering unhampered penetration, the electric current applied in TES follows the path of least resistance and is more vulnerable to the biophysical characteristics of the stimulated tissues. However, despite these important neurophysiological differences between TMS and TES, both NIBS technologies offer a variety of powerful protocols capable of reliably changing brain network activity patterns. Depending on the stimulation parameters, TMS and TES can momentarily stimulate or disrupt, but also for a longer period inhibit or facilitate local brain regions by increasing or decreasing cortical excitability respectively. In this sense, both techniques can be used to induce longer lasting neuroplastic changes in the brain, similar to LTD and LTP-like synaptic plasticity processes (1,2).
TMS and TES are clinically effective treatments
This ability of NIBS to change excitability and even network connectivity in the targeted brain regions (networks) beyond the stimulation period itself has been the basis of the incredible successful line of research leading to the development of ever refined clinical TMS and TES protocols. These clinical protocols usually require the application of many (repetitive) TMS pulses (rTMS) or prolonged durations of TES sessions (20-30 minutes), repeated over multiple treatment sessions (20-30) across an overall therapy duration of several days to weeks (1-6 weeks). The past decade has witnessed a revolution in mental health care where such TMS and TES clinical protocols now play a vital role in regulatory care as a proven clinically effective nonpharmacological treatment alternative for various neuropsychiatric disorders (3-5). Today, NIBS has rightfully earned its place in the established range of treatment options for depression, OCD, Addiction, or Pain. Following the official recognition and approval by various regulatory bodies, TMS and TES clinics are sprouting globally, and NIBS technologies are finding their way into the offices of experienced psychiatrists, psychologists, neurologists, rehabilitation specialists. The results have in some applications been astonishing with NIBS clearly filling a clinical niche, with its combination of localized, targeted modulation of intrinsic brain mechanisms and, not less important, the often much better side effect profile as compared to medication, with generally high tolerability and very few to no side effects in most patients. Every year, new approvals are granted for new or optimized clinical applications using TMS (and in some countries also TDCS). Reimbursement of the treatment costs is now even offered by public health insurance in a growing number of countries. Following these scientific, clinical, and regulatory achievements, the number of private practises and small clinics offering TMS and/or TES services is increasing continuously worldwide.
NIBS research continues to improve treatments
Despite its official recognition and approval and subsequent worldwide adoption in clinical practise, scientific research to further improve efficacy and safety of NIBS is extremely dynamic with clinically relevant improvements of protocols and procedures being introduced continuously. In the past 3 years alone, the treatment of depression with TMS has seen several impactful innovations published in the scientific literature. These constant updates on how to optimize the clinical effectiveness of TMS therapies are often of direct clinical relevance. Take as an example the new insights and developments in where and how to best position the TMS coil on the scalp to target a specific disorder-relevant brain region (network- or circuit-based TMS). Or the increasing popularity of so-called accelerated TMS protocols, offering more than one treatment session per visit, leading to important new guidelines in how to optimally design those accelerated treatments to promote therapeutically beneficial metaplasticity (6). Or the recent introduction of alternative brain targets for treating depression outside the conventional dorsolateral prefrontal cortex, a concept closely linked to the accumulating evidence that depression is extremely heterogenous with various sub types of depression existing that require different TMS treatment approaches based on stratified psychiatry. In this context, research is currently aiming to classify patients into sub-groups, find biomarkers, or adapt protocols based on measured individual brain activity or even quantifiable TMS-induced heart rate modulations (7). In fact, even fully personalized or precision TMS treatment protocols have now been introduced where integrated systems apply TMS as a “closed-loop” therapy, dynamically adjusting the TMS pulse sequences to the simultaneously measured changes in brain activity. And even remotely supervised home-use NIBS solutions have been proposed to increase accessibility and scalability in clinical practise (8). These are just a few of the recent developments published in the past 3-5 years alone with direct relevance for clinical practise.
How to keep TMS practitioners informed?
Since the field of TMS and TES is developing so dynamically, with many new scientific publications on the one hand but also more and more colleagues throughout the world joining us in offering TMS and TES to their patients in clinical practise, we need to actively keep brain stimulation researchers and TMS practitioners connected. This is, however, far from trivial or automatic.
Most of TMS practitioners or clinicians offering TMS in clinical practice don’t have free and open access to these new scientific articles published in subscribed journals, nor do they have the time to scan the overwhelming number of new articles for scientific quality and clinical relevance. These clinical colleagues are also not always attending the scientific conferences where these new developments are presented and discussed within the community.
This leads to an undesired gap between the scientific and academic community actively working to further develop and improve the efficacy of TMS/TES on the one hand, and the clinical TMS practitioners treating patients “in the field” on the other hand. At the time of writing this article, already > 900 colleagues are following this initiative on LinkedIn.
The International Clinical TMS Certification Course LinkedIn initiative
To address this increasing gap between scientific research and clinical practice in the field of noninvasive brain stimulation, the International Clinical TMS Certification Course created a LinkedIn page, providing simple access to relevant scientific publications from the international brain stimulation literature and to inform about new developments on clinical efficacy, safety, and application expansion of TMS and TES. The explicit aim is to keep researchers, clinical practitioners, health care professionals, but also patients, informed and connected to the most relevant scientific and clinical developments in the field of TMS and TES.
We are proud and happy that an increasing number of internationally renowned experts in the field of noninvasive brain stimulation have joined forces with the International Clinical TMS Certification Course to provide the service of monitoring and scanning the scientific literature for relevant new developments, summarizing the important take-home messages of these articles in short posts, and providing also the direct link to the full publication for everyone interested. We thank the authors, publishers, and university libraries for indirectly and directly supporting this open science initiative aiming to better connect scientific research and clinical practice.
Since February 2023, everyone interested can now simply follow the International Clinical TMS Certification Course on LinkedIn to benefit from this service and to stay connected with the scientific research in the field of TMS and TES. At the time of writing this article, already > 800 colleagues are following this initiative on LinkedIn.
You can follow this initiative here.
The International Clinical TMS Certification Course also offers accredited fee-based TMS Training Courses educating clinicians and researchers worldwide about how to offer TMS as a therapy in psychiatry, neurology, and rehabilitation. Courses are offered at various locations across the world and at different times throughout the year.
References
1. de Graaf, A.T., Janssens, S.E.W. & Sack, A.T. (2021). CNS medical devices: is non-invasive brain stimulation the low-hanging fruit? Modern CNS Drug Discovery (Reinventing the Treatment of Psychiatric and Neurological Disorders), Schreiber, Rudy. (Publisher: Springer International Publishing; 2021; eBook ISBN: 978-3-030-62351-7; DOI: 10.1007/978-3-030-62351-7) 2. de Graaf, T.A., Thomson, a., Duecker, F. & Sack, A.T. (2021). CNS medical devices: the various forms of non-invasive brain stimulation and their clinical relevance. Modern CNS Drug Discovery (Reinventing the Treatment of Psychiatric and Neurological Disorders), Schreiber, Rudy. (Publisher: Springer International Publishing; 2021; eBook ISBN: 978-3-030-62351-7; DOI: 10.1007/978-3-030-62351-7) 3. Lefaucheur JP, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, Filipović SR, Grefkes C, Hasan A, Hummel FC, Jääskeläinen SK, Langguth B, Leocani L, Londero A, Nardone R, Nguyen JP, Nyffeler T, Oliveira-Maia AJ, Oliviero A, Padberg F, Palm U, Paulus W, Poulet E, Quartarone A, Rachid F, Rektorová I, Rossi S, Sahlsten H, Schecklmann M, Szekely D, Ziemann U. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014-2018). Clin Neurophysiol. 2020 Feb;131(2):474-528. doi: 10.1016/j.clinph.2019.11.002. Epub 2020 Jan 1. Erratum in: Clin Neurophysiol. 2020 May;131(5):1168-1169. PMID: 31901449. 4. Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, Cotelli M, De Ridder D, Ferrucci R, Langguth B, Marangolo P, Mylius V, Nitsche MA, Padberg F, Palm U, Poulet E, Priori A, Rossi S, Schecklmann M, Vanneste S, Ziemann U, Garcia-Larrea L, Paulus W. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol. 2017 Jan;128(1):56-92. doi: 10.1016/j.clinph.2016.10.087. Epub 2016 Oct 29. PMID: 27866120. 5. Fregni F, El-Hagrassy MM, Pacheco-Barrios K, Carvalho S, Leite J, Simis M, Brunelin J, Nakamura-Palacios EM, Marangolo P, Venkatasubramanian G, San-Juan D, Caumo W, Bikson M, Brunoni AR; Neuromodulation Center Working Group. Evidence-Based Guidelines and Secondary Meta-Analysis for the Use of Transcranial Direct Current Stimulation in Neurological and Psychiatric Disorders. Int J Neuropsychopharmacol. 2021 Apr 21;24(4):256-313. doi: 10.1093/ijnp/pyaa051. PMID: 32710772; PMCID: PMC8059493. 6. Thomson, A.C. & Sack, A.T. (2020). How to Design Optimal Accelerated rTMS Protocols Capable of Promoting Therapeutically Beneficial Metaplasticity. Frontiers in Neurology, 5;11:599918. 7. Lauren Zwienenberg, Hanneke van Dijk, Stefanie Enriquez-Geppert, Nikita van der Vinne, Richard Gevirtz, Evian Gordon, Alexander T. Sack, Martijn Arns. Heartbeat-Evoked Potential in Major Depressive Disorder: A Biomarker for Differential Treatment Prediction between Venlafaxine and rTMS? Neuropsychobiology, DOI: 10.1159/000529308, published online March 2023. 8. Paneva J, Leunissen I, Schuhmann T, de Graaf TA, Jønsson MG, Onarheim B, Sack AT. Using Remotely Supervised At-Home TES for Enhancing Mental Resilience. Front Hum Neurosci. 2022 Jun 9;16:838187. doi: 10.3389/fnhum.2022.838187. PMID: 35754763; PMCID: PMC9218567.
Read this next
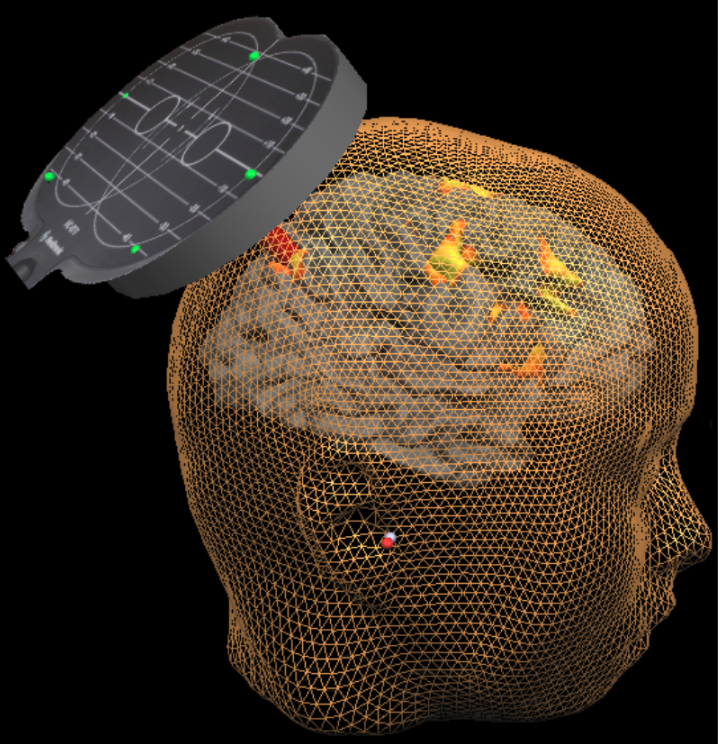
What Silicon Valley needs to know about the brain, and what it doesn't - Part I
Silicon Valley wants to get inside your head - literally. While these projects adopt mixes of commercial stealth and elaborate publicity, and the breadth of applications spans the entire human condition, all these technologies take one of two product forms: Either as a chip implanted in your head transmitting to a computer or as a wearable cap transmitting to a computer.
Neuromodulation for COVID-19, Neuromodec update 8: Encouraging news
This is the 8th update from Neuromodec (February 14, 2023) on the use of Neuromodulation for COVID-19 as part of Neuromodec’s initiative to educate on and advance treatments.
EU regulators grossly misrepresent non-invasive brain stimulation
The regulation of neuromodulation in the EU has been a muddy topic for years, and regulators recently made it all much more difficult.