The basics of Vagus Nerve Stimulation
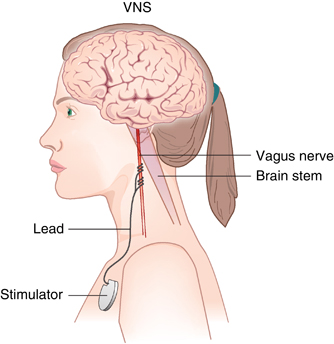
Vagus Nerve Stimulation (VNS) are medical devices that apply electrical stimulation to the vagus nerves for therapeutic purposes. The vagus nerve is a branch of the nervous system that runs from the brain, down the neck, to many organs including the heart, lungs, and digestive systems. Stimulation is applied to the vagus nerves (vagus nerve stimulation) to activate the vagus nerves which in turn activates the brain or peripheral organs.
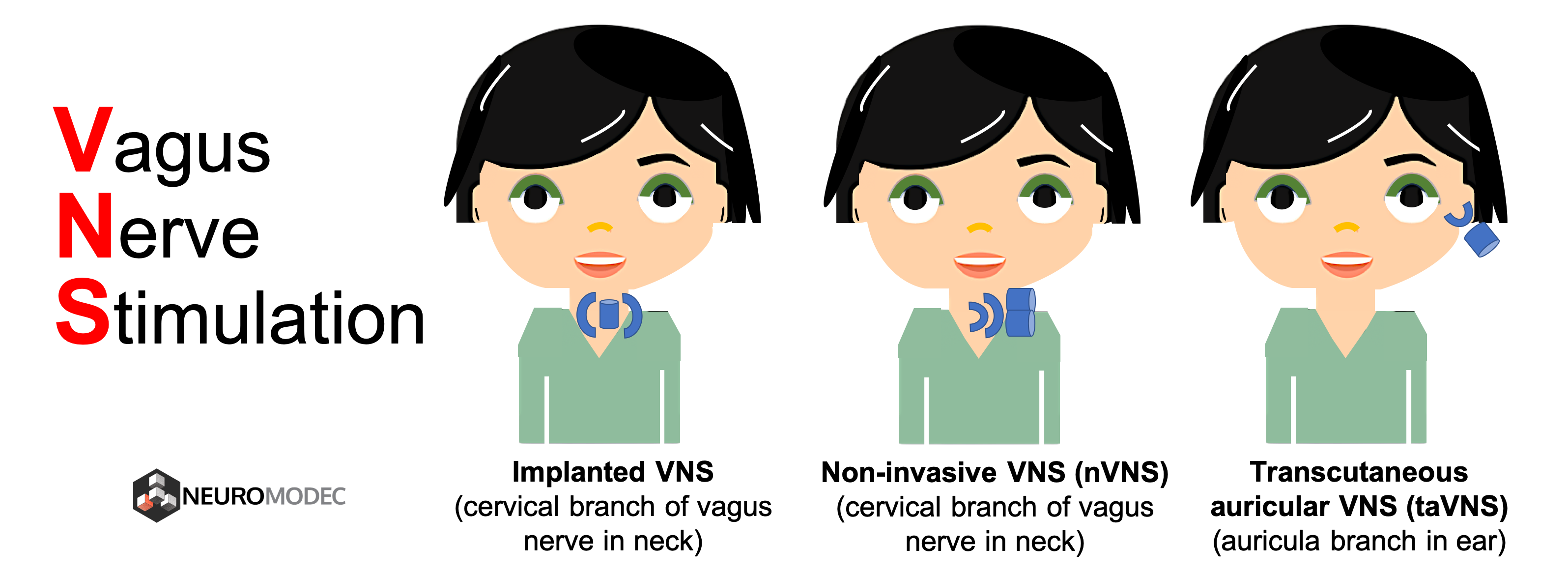
- Implanted devices which include a component inside the beck on the cervical (neck) branch of the vagus nerve. Often then the generic “VNS” is used, this is referred to as implanted cervical device. The device is on most of the time. Invasive VNS is predominantly used in epilepsy and depression, though additional applications are being explored. Every surgery is associated with risks, but after implantation the most common side-effects is temporary coughing and shortness of breath.
- Non-invasive cervical vagus nerve stimulation where a device is placed against the outside of the neck. The device is used as needed. Non-invasive cervical VNS is predominantly used in headache or migraine.
- Non-invasive stimulation of the auricular branch of the vagus nerve, which is a branch of the vagus nerves located in the ear. This approach is called transcutaneous auricular Vagus Nerve Stimulation (taVNS) and includes clip or inset placed in the ear. The device is used as needed. taVNS is investigated for many types of neurological and psychiatric disorders including epilepsy, depression, and PTSD, as well as a method to reduce inflammation, and shows promise in rheumatoid arthritis and other inflammatory diseases.

Where can I get surgical VNS Treatment?
About one-third of people with epilepsy don’t fully respond to anti-seizure drugs. Vagus nerve stimulation may be an option to reduce the frequency of seizures in people who haven’t achieved control with medications. Vagus nerve stimulation may also be helpful for people who haven’t responded to intensive depression treatments, such as antidepressant medications, psychological counseling (psychotherapy) and electroconvulsive therapy (ECT). You can use the free tool below to find doctors and clinics who provide VNS treatment. The Food and Drug Administration (FDA) has approved vagus nerve stimulation for people who: Are 4 years old and older Have focal (partial) epilepsy Have seizures that aren’t well-controlled with medications The FDA has also approved vagus nerve stimulation for the treatment of depression in adults who: Have chronic, hard-to-treat depression (treatment-resistant depression) Haven’t improved after trying four or more medications or electroconvulsive therapy (ECT), or both Continue standard depression treatments along with vagus nerve stimulation Additionally, researchers are studying vagus nerve stimulation as a potential treatment for a variety of conditions, including headaches, rheumatoid arthritis, inflammatory bowel disease, bipolar disorder, obesity and Alzheimer’s disease.
Side Effects of surgical VNS
For most people, vagus nerve stimulation is safe. But it does have some risks, both from the surgery to implant the device and from the brain stimulation. All the side effects listed below for VNS are based on the article from Mayo Clinic3.
Surgery risks
Surgical complications with implanted vagus nerve stimulation are rare and are similar to the dangers of having other types of surgery. They include:- Pain where the cut (incision) is made to implant the device
- Infection
- Difficulty swallowing
- Vocal cord paralysis, which is usually temporary, but can be permanent
Side effects after surgery
Some of the side effects and health problems associated with implanted vagus nerve stimulation can include:- Voice changes
- Hoarseness
- Throat pain
- Cough
- Headaches
- Shortness of breath
- Difficulty swallowing
- Tingling or prickling of the skin
- Insomnia
- Worsening of sleep apnea
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
References
1. Ghanem, T., & Early, S. V. (2006). Vagal nerve stimulator implantation: an otolaryngologist’s perspective. Otolaryngology-Head and Neck Surgery,135(1), 46-51. 2. Tracey, K. J. (2007). Physiology and immunology of the cholinergic antiinflammatory pathway. The Journal of clinical investigation, 117(2), 289-296. 3. Mayo Clinic Staff. (2018, December 07). Vagus nerve stimulation. Retrieved February 5, 2019, from https://www.mayoclinic.org/tests-procedures/vagus-nerve-stimulation/about/pac-20384565
